Arterial Ulcer Treatment in Los Angeles
Understanding Severe Vascular Disease


Your Vascular Partner
Dr. Michael Lalezarian
Arterial Ulcer Causes
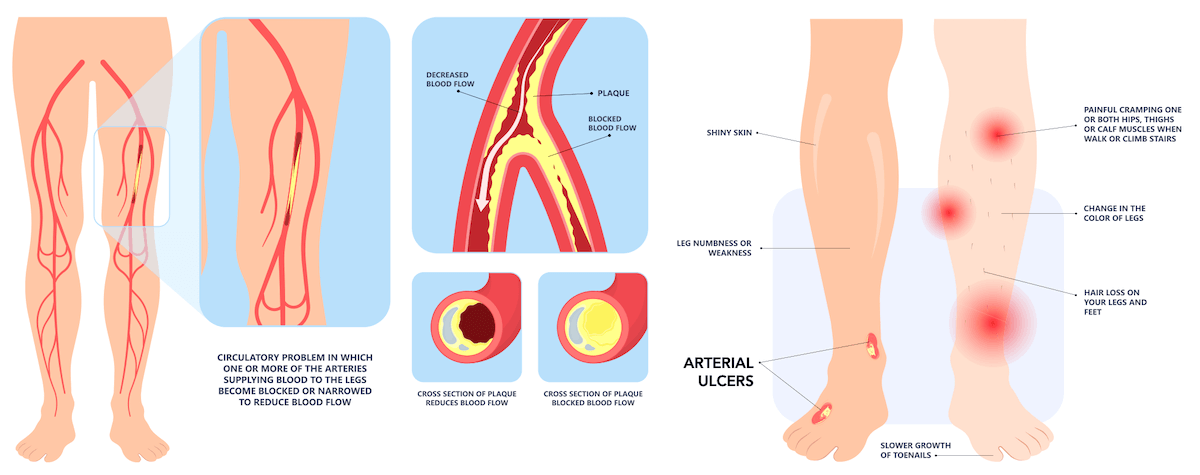
Arterial ulcers are caused by severe peripheral artery disease (PAD). Individuals with PAD experience plaque build-up in their arteries due to factors such as diabetes, obesity, high blood pressure, high cholesterol, smoking (nicotine constricts blood vessels), or other vascular diseases. This plaque accumulation and hardening of the arteries cause narrowing of medium and large arteries, limiting blood flow to the rest of the body. As a result, patients often experience muscle fatigue, leg pain, and cramping, commonly referred to as “intermittent claudication.”
As PAD worsens over time and becomes more severe, more of the arteries are affected and blood flow to the leg becomes insufficient, causing tissues to die due to the lack of oxygen. In turn, tissue death leads to ulcer formation. In many cases, an arterial ulcer persists until the underlying vascular issues are addressed.
Arterial Ulcer Risk Factors
Arterial ulcer risk factors include:
- Peripheral Artery Disease (PAD) – The primary risk factor, PAD, is caused by plaque build-up in the arteries, leading to reduced blood flow to the extremities.
- Diabetes – High blood sugar levels can damage blood vessels and contribute to the development of arterial ulcers.
- Smoking – Nicotine constricts blood vessels and accelerates plaque formation, significantly increasing the risk of arterial ulcers.
- High Blood Pressure – Hypertension can damage arteries, making them more susceptible to plaque build-up and narrowing.
- High Cholesterol – Elevated cholesterol levels contribute to plaque formation in the arteries, leading to decreased blood flow.
- Obesity – Excess weight strains the cardiovascular system and can exacerbate other risk factors like diabetes and high blood pressure.
- Older Age – Aging naturally leads to the hardening and narrowing of arteries, increasing the risk of PAD and arterial ulcers.
- Vascular Diseases – Other vascular conditions can also increase the risk of developing arterial ulcers by affecting blood flow.
Understanding these arterial ulcer risk factors is crucial for preventing arterial ulcers and managing existing conditions that contribute to their development. Despite the prevalence of these risk factors, the vascular component of arterial wounds is frequently underdiagnosed, leading many patients to live with arterial ulcers for months or even years before finding the right care.

Arterial Ulcer Symptoms
If you have an arterial ulcer, you will likely experience both peripheral artery disease symptoms and ulcer symptoms. Arterial ulcers tend to develop in specific areas of the leg / foot and have a rather distinct appearance. Below is a list of arterial ulcer symptoms and signs that may indicate an arterial ulcer:
- Leg Pain – The peripheral artery disease that causes arterial ulcers typically causes leg pain as well. PAD patients often describe an aching pain that worsens with activity and is relieved with rest, commonly referred to as intermittent claudication. In severe cases of peripheral artery disease, pain can persist even at rest.
- Ulcer Location – Over time, poor blood flow leads to skin breakdown and ulcer formation. Arterial ulcers typically occur past the point of compromised blood supply, usually at the farthest parts of the body such as the feet, toes, fingers, legs, side of the ankle, and areas of pressure to the skin.
- Ulcer Appearance – Arterial ulcers can be shallow or deep with sharp, “punched out” borders. The wound base is often pale grey or yellow and may be associated with gangrene and eschar (dry dark scab).
- Surrounding Tissue Characteristics – Tissue surrounding the arterial ulcer may be itchy, pale, shiny, red, cold to the touch, and hairless.
Arterial Ulcer Diagnosis
Diagnosing arterial ulcers involves a thorough clinical evaluation by a healthcare professional, often a vascular specialist. The diagnostic process typically includes:
- Medical History & Physical Examination – Your vascular specialist will begin by taking a detailed medical history, focusing on risk factors such as smoking, diabetes, high blood pressure, high cholesterol, and a history of peripheral artery disease (PAD). During the physical examination, the physician will assess the location, appearance, and characteristics of the ulcer, as well as the condition of the surrounding skin.
- Ankle-Brachial Index (ABI) Test – This non-invasive test measures the blood pressure at the ankle and compares it to the blood pressure in the arm. A lower blood pressure in the ankle compared to the arm suggests reduced blood flow to the extremities, indicating PAD.
- Doppler Ultrasound – This imaging technique uses sound waves to visualize blood flow in the arteries and identify any blockages or narrowing. It helps in assessing the severity and extent of the arterial disease.
- Angiography – In more complex cases, an angiography may be performed. This involves injecting a contrast dye into the blood vessels and taking X-ray images to pinpoint the location and severity of arterial blockages.
- Blood Tests – Blood tests may be conducted to check for underlying conditions such as diabetes, high cholesterol, and other factors contributing to poor arterial health.
- Skin Biopsy – In rare cases, a small sample of skin tissue from the ulcer may be taken for laboratory analysis to rule out other causes of non-healing wounds, such as infections or malignancies.
By combining these diagnostic tools, the vascular specialists at ProVascularMD can accurately diagnose arterial ulcers and develop an effective treatment plan tailored to your specific needs. Early diagnosis and intervention are key to preventing complications and promoting healing.
Arterial Ulcer Treatment
Lifestyle Changes & Medical Management
Arterial Wound Care
Patients with open, non-healing arterial wounds are typically referred to an arterial wound care specialist who will clean the wound routinely and dress it with bandages to prevent infection and promote healing. Although wound dressing changes do not target the underlying arterial disease, arterial wound care is still an essential part of healing and complements other treatments.
Minimally Invasive Revascularization
Surgical Options
For severe arterial disease that cannot be addressed with minimally invasive techniques, more invasive surgical options are available. These can include arterial bypass surgery, endarterectomy, and even amputation surgery in extreme cases.
Before & After Arterial Ulcer Treatment
The image below shows how minimally invasive revascularization can heal arterial ulcers by restoring blood flow to the affected area.

Don’t Let Your Arterial Ulcer Go Untreated
Your Partner in Vascular Care
Lower Extremity Arterial Disease
Peripheral Arterial Disease Treatment
What Are Arterial Ulcers?
Vascular Specialist in Los Angeles
Learn more about Los Angeles Vascular Specialist Dr. Michael Lalezarian.
Schedule Your Visit
Click the Chat Button
Vascular Care in Los Angeles
& San Bernardino County
Adelanto
Alhambra
Amboy
Angelus Oaks
Apple Valley
Arcadia
Azusa
Baker
Baldwin Park
Barstow
Bell Gardens
Big Bear City
Big Bear Lake
Bloomington
Blue Jay
Bryn Mawr
Burbank
Cedar Glen
Cedarpines Park
Chino
Chino Hills
Cima
Citrus
City of Industry
Claremont
Colton
Covina
Crestline
Daggett
Diamond Bar
Downey
Duarte
Eagle Rock
Earp
El Monte
Essex
Fawnskin
Fontana
Forest Falls
Fort Irwin
Glendale
Glendora
Grand Terrace
Green Valley Lake
Guasti
Hacienda Heights
Helendale
Hesperia
Highland
Highland Park
Hinkley
Irwindale
Joshua Tree
La Canada
La Crescenta
La Habra
La Mirada
La Puente
La Verne
Lake Arrowhead
Landers
Loma Linda
Lucerne Valley
Ludlow
Lytle Creek
Mentone
Monrovia
Montclair
Montebello
Monterey Park
Morongo Valley
Mountain Pass
Mt Baldy
Needles
Newberry Springs
Nipton
Norwalk
Ontario
Oro Grande
Parker Dam
Pasadena
Phelan
Pico Rivera
Pinon Hills
Pioneertown
Pomona
Rancho Cucamonga
Redlands
Rialto
Rimforest
Rosemead
Running Springs
San Bernardino
San Dimas
San Gabriel
Santa Fe Springs
Sierra Madre
Skyforest
South El Monte
South Pasadena
Sugarloaf
Temple City
Trona
Twentynine Palms
Twin Peaks
Upland
Victorville
Vidal
Walnut
West Covina
West San Dimas
Whittier
Wrightwood
Yermo
Yucaipa
Yucca Valley




